Introduction to ECGs
Introduction to ECGs
The heart muscle contracts because of a precise sequence of electrical impulses that travel through it in a predictable pattern. We have a very good understanding of what this “normal” electrical conduction looks like. Many cardiac pathologies, from heart attacks and heart blocks to valve problems, can alter this sequence.
The surface electrocardiogram, commonly called an ECG or EKG, is a non-invasive test that visualizes and records this electrical activity. (The term EKG comes from the original Dutch “elektrokardiogramm,” coined by Dr. Willem Einthoven, who is considered the father of modern electrocardiography.) The test works by placing electrodes (conductive pads) on the skin to detect the heart’s tiny electrical signals. An ECG machine then measures the voltage difference between these electrodes over time, displaying it as a graph. By analyzing the shape, size, and timing of the waves on this graph, we can gain incredible insight into the heart’s condition.
The first instrument capable of accurately recording the heart’s electrical activity was the string galvanometer, invented by Dr. Einthoven in the early 1900s. Instead of today’s familiar stickers, this massive machine used buckets of saltwater as electrodes. It was with this device that we first appreciated that the normal heart had a regular, repeating electrical pattern.
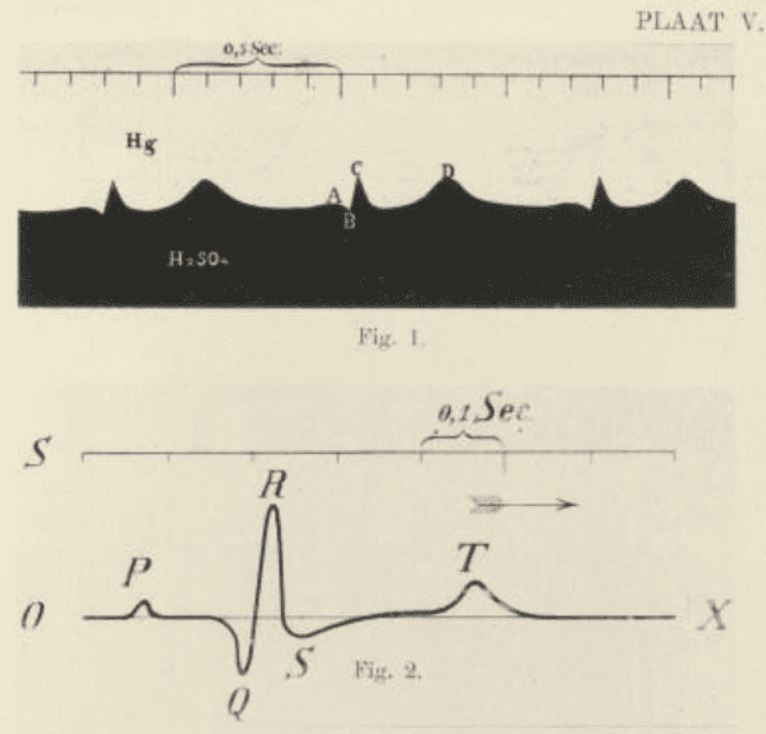
Einthoven found that each heartbeat was associated with a series of distinct electrocardiographic “waves”, which he went on to label as the P, Q, R, S, and T waves, a convention that persists to this day.
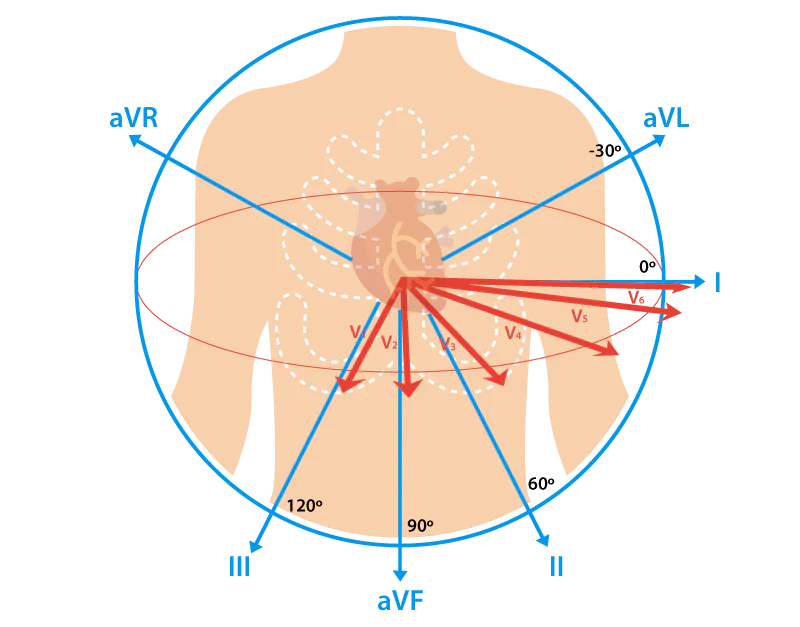
As the technology evolved, it became clear that different arrangements of electrodes allowed us to view the heart’s electrical activity from different angles, much like having multiple cameras on a single subject. Each of these perspectives, created by measuring the voltage between a pair of electrodes, is called a lead. The standard modern ECG incorporates 12 different leads to create a comprehensive, multi-faceted view of the heart, which is essential for accurate diagnosis.
Because different cardiac problems manifest in different ways, we use several ECG recording methods:
This provides a comprehensive snapshot of the heart’s electrical activity, typically over 10 seconds. It is excellent for identifying persistent issues, such as structural changes like left ventricular hypertrophy or cardiomyopathy. It can also reveal the cardiac effects of systemic issues, like electrolyte abnormalities, drug influences, or non-cardiac diseases.
There are also variations on this idea, and by changing the position of the electrodes, you can generate more “leads” and more perspectives to look at the heart. These non-standard views, such as posterior or right sided leads, are used in specific clinical situations to provide additional diagnostic information that is not available from the standard 12 leads. We’ll get into all of this in more detail later.
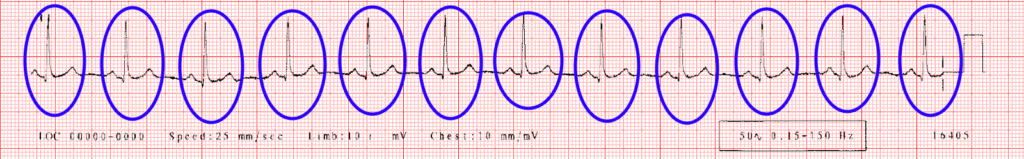
Some conditions, like myocardial ischemia, can cause dynamic, evolving changes in cardiac electrical activity. In these cases, we perform serial 12-lead ECGs to track these changes over time. This principle is also the basis for the exercise stress test, where an ECG is recorded while a patient exercises on a treadmill to see if physical stress induces any ischemic changes.
Sequential ECGs showing development of ischemic changes with treadmill exertion.
To assess abnormal heart rhythms (arrhythmias) that may be infrequent (or at least infrequent enough that they might be missed on a 10 second snapshot), we need to monitor the ECG over a longer duration. We don’t always need all 12 leads, and often just one or two leads might suffice to tell us what is happening (although it’s never bad to have more information). A few examples of rhythm monitoring: